Alcohol abuse is common in the United States with 14.1 million adults estimated to have some degree of alcohol use disorder. Emergency physicians will encounter this quite often, either as the primary presenting problem or as a complicating factor in a patient’s care. Unfortunately, alcohol consumption appears to be increasing, with the World Health Organization projecting ongoing increases through at least 2025. As a result, it is becoming increasingly important that we understand the serious and potentially life-threatening consequences of alcohol withdrawal syndrome (AWS) and the treatment options that exist in order to best manage these patients. The following three journal club articles sought to investigate potential clinical benefits for the use of phenobarbital in the emergency department (ED) for the treatment of AWS.
Recent data from the National Center for Health Statistics reveal that in the 12-month period ending in April 2021, more than 100,000 Americans died of an overdose, a staggering increase of nearly 30% the prior year. While the ongoing COVID-19 pandemic has contributed to overdose deaths and taxed constrained ED resources, it has also clarified the important role that emergency physicians have in expanding access to life-saving medications to treat opioid use disorder. In this journal club, we review the evidence on ED-initiated buprenorphine, including barriers to implementing ED-buprenorphine here in rural Maine.
Suicide is disturbingly prevalent among patients we care for in the Emergency Department. It is unfortunately also common among physicians. Most estimates suggest that approximately 400 physicians die by suicide annually. Physicians also have a higher rate of suicide than the general population. Male physicians have a 40% increased risk of suicide compared to their age-matched peers and female physicians have a 130% increased risk. We chose this topic for Journal Club with the goals to raise awareness around these shocking statistics, discuss etiologies behind these high rates of suicide and to normalize the discussion around physician mental health.
Renal colic is a commonly encountered diagnosis in the emergency department that is known to cause significant pain. In clinical practice, the initial goal is prompt pain management while simultaneously working to confirm the suspected diagnosis. Because of the severity and acuity of the pain associated with renal colic, opioid pain management has often been used. Given the overall goal of reducing the use of opioid pain medications, emergency physicians have been working to identify alternative pain management strategies with agents such ketorolac and lidocaine. In this journal club, we examine the evidence in support of these treatment strategies.
On January 23rd, 1849 Elizabeth Blackwell became the first female graduate of a US medical school, graduating from Geneva College in New York as the Valedictorian of her class. Despite the passage of 172 years from that remarkable moment, female physicians continue to face both implicit and explicit gender bias within the medical profession and culture. This journal club examined the impact of gender bias on female emergency medicine trainees.
The use of TXA in the care of the trauma patient has become prevalent since the publication of the MATTERs and CRASH-2 studies which demonstrated significant mortality benefits in trauma patients who received early TXA after admission. Since these publications, there continues to be several additional questions regarding its TXA: 1) If earlier treatment with TXA for the trauma patient is better, would there be benefit in its administration in the prehospital setting? 2) Is there benefit to the use of TXA in patients with TBI to prevent the progression and subsequent morbidity and mortality? 3) Lastly, does TXA carry a significant risk for side effects, including venous thromboembolic events? This journal club reviewed four articles that aim to answer these questions.
COVID vaccines have dominated the media and our recent efforts to combat the SARS-CoV-2 virus. It will likely take some time, however, until we reach herd immunity. To help curb the severity of disease, the medical community continues to investigate other therapeutics. By examining the virus life cycle and our immune system’s response to it (both protective and destructive), we may be able to develop anti-viral and immune therapy that counteracts the cytokine storm and leads to acute respiratory distress syndrome, respiratory failure, shock, organ failure and potentially death. In this journal club, we reviewed the use of steroids and convalescent plasma for the treatment of patients with SARS-CoV-2.
Vasopressors are used in Emergency Medicine to treat cardiac arrest, hypotension, and shock. Recent studies have sought to investigate questions around timing, medication choices, and administration of these medications in varying clinical scenarios. The emergency provider must be familiar with the properties of, and indications for, vasopressors in the ED setting. In this journal club summary, we review the evidence on the impact vasopressors have on clinical outcomes.
Despite the widespread prevalence of concussions, little is known about its ideal management. The traditional recommendation for concussion treatment has centered around the concept of “brain rest” in addition to physical rest. There is little medical evidence to support this recommendation. Our journal club sought to answer whether some physical activity could actually benefit patients with acute concussion and additionally reviewed a study (completed in Maine) that challenged the belief concussions have long term cognitive effects. Read on to see what you think!
April’s journal club looked at four clinical questions regarding the diagnosis and expectant course of renal stones. Can the STONE score help you determine if your patient’s flank pain is due to a renal stone? Which is better to confirm your clinical suspicion of a renal stone, ultrasound or CT? How likely will your patient’s kidney stone pass spontaneously? What is the accuracy of hematuria to predict a renal stone in the patient with flank pain?
The evaluation of a child for non-accidental trauma (NAT) is an infrequent, yet high risk endeavor for emergency physicians. Abusive head injury is the most common cause of death in cases of non-accidental trauma and up to 30% of cases of child maltreatment are misdiagnosed at first health care contact. There is a growing body of literature that helps to frame the workup and risk stratification of children at risk for NAT. This month’s journal club focused on 3 articles centered on risk factors and diagnosis of abusive injuries.
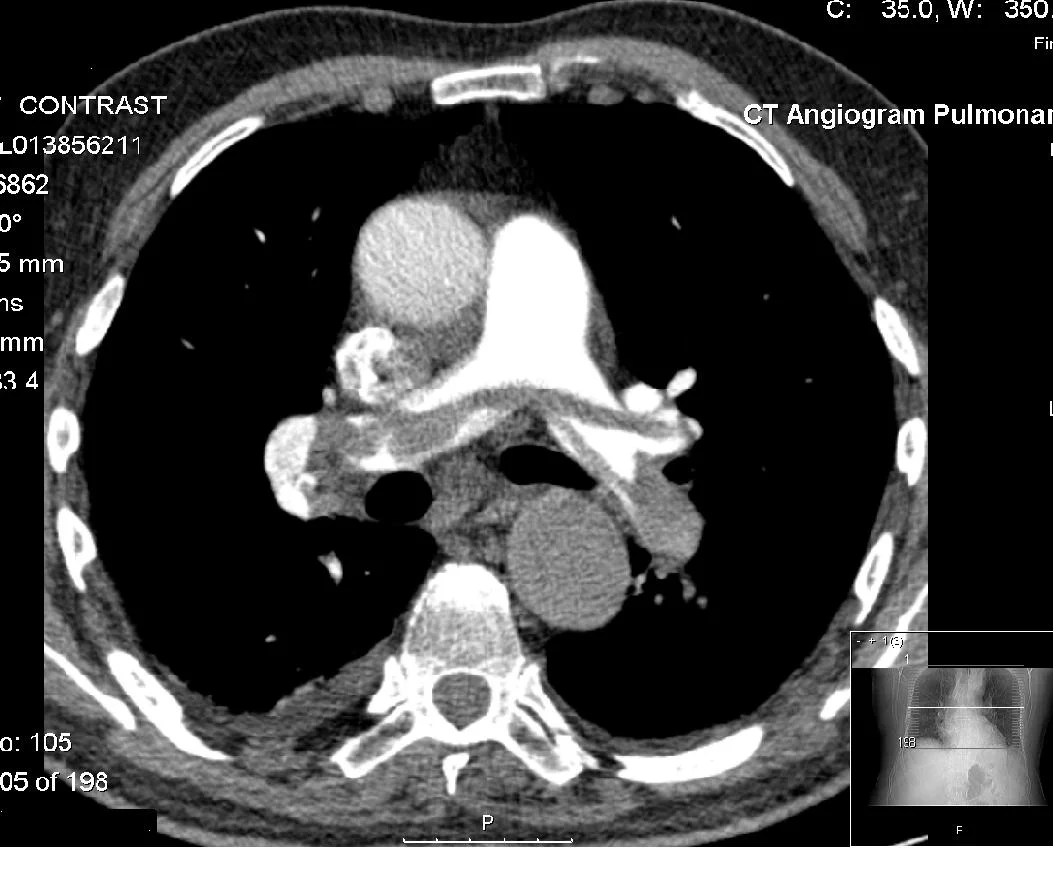
Computed tomography (CT) is a commonly used imaging modality in the US. In 2013, greater than 74 million CT scans were ordered. Although recently there has been a decrease in the need for contrast for certain diagnostic needs, contrast remains very important in the diagnosis of pulmonary embolus, aortic pathology, infectious processes, and other soft-tissue pathology. Acute kidney injury (AKI) has been a concern for many years and the teaching has been that contrast can increase the risk of acute kidney injury. Recent literature has addressed this issue and this month’s journal club offers a synopsis of these articles.
Geriatric patients (> age 65) account for almost 1 in 5 of all cervical spine fractures, with 50% of cervical spine fractures occurring at the C1/C2 level. Recent literature has questioned whether these clinical decision rules may be applied in the geriatric population, where over half of identified cervical spine fractures result from ground level falls. Furthermore the reliability of physical exam, specifically midline tenderness, has been questioned in elderly patients. January's journal club examined three articles that addressed this specific population of blunt trauma patients at risk for cervical spine injury.
Ischemic stroke is one of the most frequently encountered neurologic emergencies. It can be a truly debilitating diagnosis, and yet classically, there has only been one treatment available for small and large vessel occlusions alike– tPA. Now, with the widespread availability of CT angiography and the advent and maturation of interventional techniques such as mechanical thrombectomy, the management of large vessel occlusion (LVO) strokes is rapidly evolving and is increasingly distinct from the management of other strokes. This is truly an exciting time in stroke care, so for this month’s journal club we focused on three questions relevant to the emergency provider: 1) What is the utility of prehospital clinical scales for rapidly identifying LVO strokes? 2) Should patients with suspected LVO be taken to the nearest stroke center or bypass smaller hospitals to reach a comprehensive stroke center? 3) How effective is mechanical thrombectomy vs. tPA alone?
Low back pain is one of the most common emergency department presentations. Though diagnosis is often straightforward, pain management can be a source of frustration for both the patient and the provider, especially as we focus on limiting narcotic prescriptions given the spreading opiate crisis. In an effort to manage pain, practitioners often counsel patients on the use of over the counter medications or discharge them with a prescription, but what is the evidence behind these medications that we commonly use for back pain? For this month’s journal club, we reviewed three articles that studied the use of acetaminophen, NSAIDS plus muscle relaxers or opiates, and corticosteroids for the management of acute low back pain.
Angioedema (non-pitting edema of submucosal tissues) results in infrequent, but high-risk emergency department visits. Since airway edema can make oropharyngeal and nasopharyngeal intubation impossible, our focus is on early and aggressive pharmacologic treatment to prevent life threatening airway obstruction. Recall that angioedema can come from two broad physiologic mechanisms: histamine mediated (ie allergic in nature which may have urticaria or other evidence of anaphylaxis) or bradykinin mediated (eg hereditary angioedema, ACE-induced angioedema). Histaminergic mediated typically responds well to aggressive antihistamines, steroids, and epinephrine. Bradykinin mediated, however, does not. This month we focused on this type of angioedema that can be non-responsive to our typical first line therapies.
Cellulitis is commonly treated in the emergency department. Patients who present with cellulitis incur significant health care costs and may be over-treated with antibiotics. For our August journal club, we selected articles that would help providers avoid treatment errors that lead to high costs, unwanted side effects, overuse of antibiotics and unnecessary admissions.
With nearly 1 million US emergency department (ED) visits attributed to acute heart failure (AHF) annually, heart failure is a serious illness frequently managed by emergency physicians. More than 80% of visits result in hospital admission, and readmission rates may range from 30-60% within 3 to 6 months of initial discharge. ED visits related to AHF are expected to continue to rise with the aging population and improved survival rates in patients with chronic heart failure and acute coronary syndromes. One critical issue facing emergency physicians caring for AHF patients is deciding upon disposition: admission (with or without monitoring) or discharge (with or without early follow-up). Consensus guidelines are available to support decision-making around diagnosis and treatment; however, no current guidelines provide an evidence-based approach to disposition. For this month’s journal club, we reviewed three papers examining decision aids developed to assist emergency physicians in determining risk in AHF patients.
Emergency physicians regularly see psychiatric patients who are having suicidal thoughts or engage in non-suicidal self-injurious (NSSI) behavior. In addition to working these patients up medically, it is part of our job to determine who needs emergent evaluation by a psychiatric provider and who is safe for discharge. This is a very important decision, as we do not want to send high risk patients home and keep low risk patients for extended periods of time while they await their evaluation. Balancing this can be difficult - oftentimes it is not obvious where a patient falls on this spectrum. We are taught various decision aids in medical school to help us risk stratify these patients - but how do they perform on emergency department patients? For this month's journal club, we looked at three papers that examine three different decision aids to help elucidate this issue.
Urinary complaints in females are an incredibly common reason for visits to emergency departments. We are often left to make the decision of whether to treat for infection on fairly equivocal urinalysis results without the help of a definitive culture. Muddying the waters is the risk of sexually transmitted infections (STI's) which can cause similar if not more benign symptomatology (even at times completely asymptomatic). Can the history help? Do reported symptoms correlate with a diagnosis? In April's journal club, we chose articles that aimed to clarify the distinction between two entities (UTI vs. STI) that are incredibly frequent in sexually active women.
The availability of herbal and dietary supplements in the U.S. is increasing exponentially: 4,000 in 1994 to 80,000 today. Half of all adults have reported using at least one dietary supplement in the past month, but many do not openly relay this to their primary care physicians or emergency medicine physicians. This month’s journal club focused on the utilization of these products, their adverse events/complications as well as their “regulation”.
Since Prandoni et al published their findings in the NEJM's October 2016 issue (reporting a 17.3% incidence of pulmonary embolism among patients admitted with first time syncope), there has been controversy swirling in the EM community. Questions have been raised regarding the impact of this study, its generalizability, and its implications for clinical practice. At this month’s journal club, we broke down the findings in the Prandoni study as well as looked at two other studies (Castelli et al and Altinsoy et al) that examined the clinical characteristics of patients with PE who presented with syncope.
At this journal club we looked at a number of studies examining the concept. While they were of varied design, the premise of all was the same; namely with an antibiotic only approach, what is the success rate, recurrence rate, and cost savings / loss?
This month Dr. Rappold opened up his home to us where we discussed the utility of bedside ultrasound and plain films in the resuscitation of the trauma patient.

































In the United States, racism is a critical public health problem, permeating everyday systems including educational and health care systems; criminal justice and legal systems; financial, housing, and economic systems; environmental issues and beyond to create differential health outcomes that adversely affect Black, Indigenous, and other people of color. This pervasive system of power is based on the socio-politically constructed notion that non-Hispanic white people are inherently superior to people of color (Black, African American, Indigenous, Native American, Alaska Native, Native Hawaiian, Pacific Islander, Asian, Latine, Hispanic) and this ideology operates across multiple levels (individual, interpersonal, institutional) to unjustly advantage non-Hispanic white people, unjustly disadvantaging people of color. We recognize that racism is an important cause of health disparities and that, as health care providers, we have a responsibility to educate ourselves about racism so that we will be prepared to acknowledge the impact of racism on our patients’ health and work towards more equitable systems in support of health equity. One important component of that education is learning how to engage in productive conversations about race and racism. In service of that goal, we chose Ijeoma Oluo’s book, So you want to talk about race, as our common read for this special Journal Club session.