Combating the Crisis - Not Your Osler's Endocarditis Anymore
/IV drug use (IVDU) is on the rise, along with those diseases which occur from its use (osteomyelitis, septic arthritis, endocarditis, skin and soft tissue infections, spinal epidural abscess). Until we can turn the tide of the opiate wave, we must be able to diagnose and treat the diseases that occur from IVDU. We are excited to introduce a new series of educational posts dedicated to helping the emergency provider care for patient with opiate addiction. In today's inaugural post we review the contemporary epidemiology of infective endocarditis and its association with IVDU.
BACKGROUND
- Sir William Osler was a Canadian physician who made a significant contribution to our modern knowledge of infective endocarditis.
- His gulstonian lectures at the Royal College of Physicians on 'ulcerative endocarditis' appeared in Lancet in 1881 and are regarded as the most important contribution pertaining to the field of infective endocarditis. They were based on his personal experience which included more than 200 patients with clinicopathologic correlation.
- The classical patient with infective endocarditis described by Dr. Osler and textbooks no longer represents the majority of cases in practice.
- The emergence of staph infections, indwelling devices, culture negative endocarditis and intravenous drug use (IVDU) are just a few of the factors making the diagnosis and treatment as great a challenge as ever.
“Few diseases present greater difficulties in the way of diagnoses than malignant endocarditis, difficulties which in many cases are practically insurmountable. It is no disparagement to the many skilled physicians who have put their cases upon record to say that, in fully one-half the diagnosis was made post mortem.”
THE CURRENT OPIOID CRISIS
- Pick whatever statistic you like, they are staggering:
- 91 Americans die every day from opioid abuse
- 770,000 IV drug users (IVDU) in USA in 2017
- Heroin is cheaper than a pack of cigarettes in many states.
- Until we can gain some traction in fighting this crisis, we must be able to detect and treat the complications from this addiction.
THE CHANGING FACE OF IE
- Increasing IVDU is changing the demographic and clinical factors of IE
- Demographic factors among IVDU IE patients are making it harder to detect and treat
- More homelessness
- More incarceration
- Increase in underinsured/uninsured
- Higher rates of refusing medical advice
- High recurrence rate due to medical non-compliance and continuing IVDU
- Difficulty with lifelong anticoagulation compliance for bioprosthetic valves
- Increase in IVDU means an increase in right sided endocarditis only (up to 64% in some studies)
THE DIFFICULTY WITH RIGHT SIDED IE
- Murmurs are frequently inauduble
- Peripheral embolic phenomena are rare
- Duke Criteria sensitivity weakened
- Embolic phenomena represent minor criteria in the modified Duke system, but are less commonly found in right sided IE
- Right sided IE have less embolic clues
- While left sided IE can embolize to the brain, eyes, kidney, spine, joints, etc., right sided IE embolizes only to the lung
HOW DO WE CATCH THESE CASES OF RIGHT SIDED IE?
- Start with a solid history and physical exam
- Listen very carefully for a murmur (but do not depend upon it)
- Look for hematuria, splenomegaly
- Examine your patients for embolic and immunologic phenomena (Roth spots, Janeway Lesions, splinter hemorrhages, Osler nodes)
- Consider risk factors such as IVDU, recent instrumentation or procedures, indwelling lines, hemodialysis, history of rheumatic heart disease, or degenerative valvular problems.
- Screen for signs and symptoms of IE in IVDU patients when they present with other complaints (skin and soft tissue infections, overdose, etc)
- Pick off the low hanging fruit
- Fever and stroke equals IE until proven otherwise
- Multiple sites of infection equals IE until proven otherwise
- IVDU plus bacteremic infections (e.g. spinal infections) equals IE until proven otherwise
- Scrutinize the lungs – they are your “window to the heart”
- 50% of right sided IVDU have evidence of septic pulmonary emboli on chest xray
- Scrutinize the chest xray for signs of pneumonia (especially multifocal pneumonia), cavitary lesions, empyema, or effusion
- Multiple cavitary lesions should be assumed to be secondary to IVDU until proven otherwise
- Have a low threshold to order a CT chest for suspicious findings on a chest xray
DIAGNOSING RIGHT SIDED IE
- It would be nice to have an ED decision instrument that can reliably determine which febrile IVDU patients have IE.
- This would lead to considerable resource savings over the current practice of routine admission.
- Unfortunately there are no good ED protocols to decide who to admit.
- The diagnosis of IE is based on clinical, microbiologic and echocardiographic findings.
- There are numerous tests one could order that can increase or decrease your suspicion of the disease (CBC, CRP, ESR, BNP, EKG, etc) but the cornerstone tests are blood cultures and formal echocardiography.
BLOOD CULTURES
- Have a low threshold to order blood cultures in the patient you suspect has IE (even without a fever!)
- Numerous societies have differing recommendations on blood cultures
- At minimum, get 3 blood cultures from 3 different sites, with an hour between the first and third blood culture
- Three cultures has been shown to be > 90% sensitive
ECHOCARDIOGRAPHY
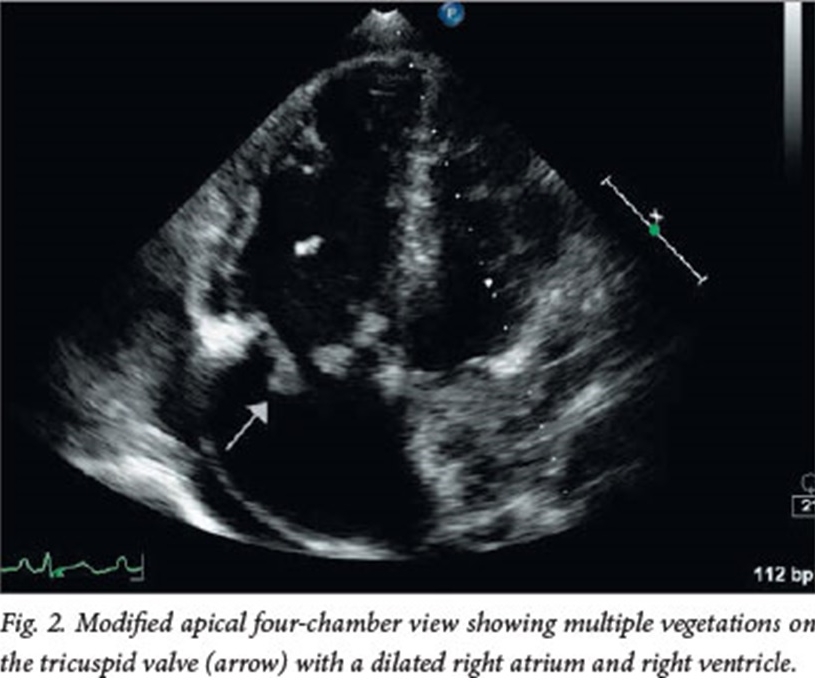
- Point of Care Ultrasound Echocardiography can help rule in IE but certainly does not rule it out – if you have a high clinical concern for the diagnosis, admit your patient for cultures and formal echocardiography.
SUMMARY
- The face of infective endocarditis is changing - today's demographic and clinical factors are making it harder to diagnose and treat.
- Right sided endocarditis requires clinical vigilance due to decreases sensitivity of the history, clinical exam and diagnostic criteria.
- The lungs are the window to the heart - pay special attention to your lung exam and radiography for clues to right sided endocarditis.
- Blood cultures and echocardiography are the cornerstones of testing.
Tired of reading? Watch Dr. Holmes discuss the changing face of endocarditis
References
1. Ronan, MV et al. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Aff (Milwood) 2016; 35:832-7. [Pubmed]
2. Wurcel AG et al. Increasing infectious endocarditis admissions among young people who inject drugs. Open Forum Infect Dis 2016. [Pubmed]
3. Hartman L, et al. Opiate injection – associated infective endocarditis in the Southeastern United states. AM J Med Sci 2016; 352: 603-8. [Pubmed]
4. Yuan SM. Right sided infective endocarditis: recent epidemiologic changes. Int J Clin Exp Med 2014; 7: 199-218. [Pubmed]
5. Cooper et al. Nationwide increase in the number of hospitalizations for illicit injection drug use-related infective endocarditis. Clin Infect Dis 2007; 45: 1200-3.[Pubmed]
6. Bonow RO, et al. Braunwald’s heart disease: a textbook of cardiovascular medicine. 9th edn. Philadelphia, PA: Saunders Elsevier, 2011. [Elsevier Link]
7. Miro et al. Infective endocarditis in IV drug abusers and HIV-1 infected patients. Infect dis clin North Am 2002; 16: 273-95, vii-viii.[Pubmed]
8. Haverkos HW, et al. Serious Infections other than Human Immunodeficiency virus among intravenous drug abusers. J Infect Dis 2000; 30: 633-8.
9. Moss R, Munt B. Injection drug use and right sided endocarditis. Heart 2003; 89: 577-81. [Pubmed]
10. Rodriguez R, et al, A pilot study to develop a prediction instrument for endocarditis in injection drug users admitted with fever. Am J of Emerg Med (2011) 29, 894-898.[Pubmed]
11. Asgeirsson H, et al. Low mortality but increasing incidence of Staphylococcus aureus endocarditis in people who inject drugs. Medicine (2016) 95:49. [Pubmed]
12. Watkins RW, Lang S, Lambert PA, et al. The Microbiologic Diagnosis of Infective Endocarditis. J Infect 2003: 47: 1-11. [Pubmed]
13. Lansky A, et al. Estimating the number of persons who inject drugs in the United States by meta-analysis to calculate national rates of HIV and hepatitis C virus infections. PLOS ONE. 2014;9(5). [Pubmed]
14. DeRosa F.G, et al. Infective Endocarditis in Intravenous Drug Users from Italy: the Increasing Importance in HIV-infected Patients. Infection 35, 2007, no. 3. [Pubmed]
15. Baddour LM, et al; American Heart Association Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease of the Council on Cardiovascular Disease in the Young, Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and Stroke Council. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association.Circulation. 2015 Oct 13;132(15):1435-86. [Pubmed]
Written and posted by Jeffrey A. Holmes, MD