What the Heck is Going on with this Pacemaker?!
/Pacemakers and implantable cardioverter/defibrillators (ICDs) are fascinating little machines. They were first placed in surviving victims of sudden cardiac death in 1980, and over the past several decades have become more complex with increasing abilities to sense, pace and defibrillate. As the population ages and the prevalence of cardiovascular disease increases, patients with pacemakers and ICDs will present more commonly to the emergency department. It is imperative that the emergency provider have a framework for troubleshooting these devices. This post will briefly review the use of the "donut" with an implantable pacemaker, as well as three pacemaker malfunctions the emergency provider may encounter.
WHAT HAPPENS WHEN YOU PLACE A MAGNET ON A PACEMAKER?
The magnet turns the sensing function of a pacemaker off and sets the pacer to a preprogrammed asynchronous mode (usually 70-90 bpm)
Application of the magnet allows for:
Assessment of pacemaker capture (but not sensing)
Evaluation of battery life
Treatment of pacemaker-mediated tachycardia
Assessment of pacemaker function when the native heart beat is greater than the pacing threshold
Red arrows signal native atrial beats, followed by ventricular pacer spike and pacer stimulated ventricular complex; after the magnet applied, the sensing function of the PM is turned off; green arrows demonstrate asynchronous atrial and ventricular pacer spikes
CLINICAL SCENARIO #1 - FAILURE TO PACE
Definition: Pacemaker fails to deliver an electrical stimulus
EKG: No pacer spikes
This Patient with a history of Complete heart block and an AICD has no pacer spikes on his ECG
CAUSES OF FAILURE TO PACE:
Pacemaker Isn’t Working
Component/battery failure
Lead problem
Electromagnetic interference (eg. MRI)
Pacemaker is being told not to fire (over sensing, the most common cause of failure to pace)
Pacemaker senses skeletal myopotentials as intrinsic cardiac activity (eg. Sit ups, push ups, mycolonic activity after succinylcholine administration)
Large T or U waves misinterpreted by the pacemaker as native QRS complexes
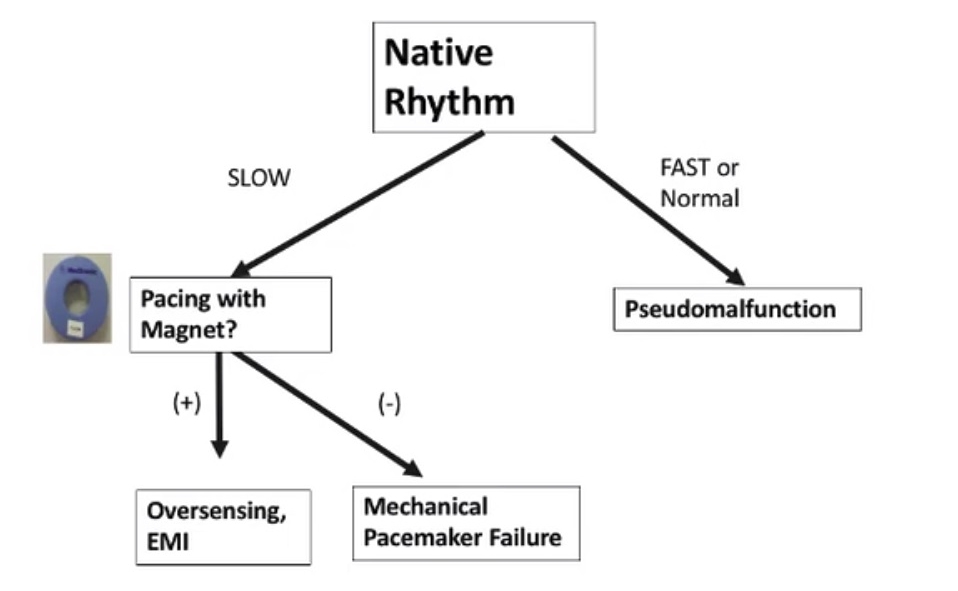
How you troubleshoot failure to pace?
cLINICAL sCENARIO #2 - FAILURE TO CAPTURE
Definition: Pacemaker stimulus fails to cause depolarization
EKG: Pacer spike without resultant P or QRS
CAUSES OF FAILURE TO CAPTURE:
Pacemaker Problem (Lead dislodgement, lead fracture, battery depletion)
Myocardial Problem/change in the depolarization threshold (exit block, acute MI, metabolic, medications)
How do troubleshoot failure to capture?
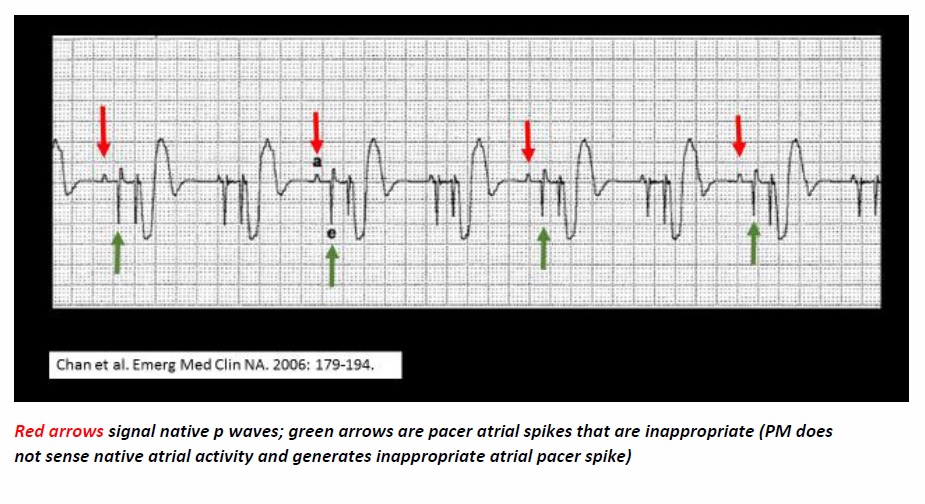
CLINICAL sCENARIO #3 - Failure to Sense
Definition: Pacemaker fails to detect, or sense, native cardiac activity and generates an
inappropriate pacer spike
EKG: Pacer spike present despite native P or QRS complex
CAUSES:
Pacemaker problem (lead problem, battery End of life)
Metabolic/electrolyte abnormality
External defibrillation
Intra-cardiac signal changers (eg. bundle branch block)
Intra-cardiac signal occurs during pacemaker refractory period
Iatrogenic (magnet – turns off sensing function)
How do you troubleshoot failure to sense?
Tired of Reading? Watch Dr. Holmes discuss the rogue pacemaker at the 2017 Maine medical Center Winter Symposium
References
1. Chan TC, Cardall TY. Electronic Pacemakers. Emeg Med Clin N Am 2006: 24: 179-94.
2. Harper RJ, Brady WJ, Perron AD, et al. The Paced electrocardiogram: issues for the emergency physician. Am J Emerg Med 2001; 19:551-60.
3. Passman R, Kadish A: Sudden death prevention with implantable devices. Circulation.116:561 2007
4. Sarko JA, Tiffany BR. Cardiac pacemakers: Evaluation and management of malfunctions. Am J Emerg Med 2004; 18: 435-40.
Written and Posted by Jeffrey A. Holmes, MD